 Since the launch of World Alzheimer's Month in 2012 by Alzheimer's Disease International, the prevalence of this disease has continued to climb. Today, approximately six million US patients are living with the disease. By 2050, an estimated 13 million people in the US will be afflicted with Alzheimer's disease (AD)1.
Since the launch of World Alzheimer's Month in 2012 by Alzheimer's Disease International, the prevalence of this disease has continued to climb. Today, approximately six million US patients are living with the disease. By 2050, an estimated 13 million people in the US will be afflicted with Alzheimer's disease (AD)1. While the number of new cases per 100,000 is on the decline, due to better understanding of the disease risk factors, the number of people with Alzheimer's is projected to grow simply because the number of adults aged 65 and over (the target group most at risk for the disease) is rising rapidly1.
The Characteristics of Alzheimer's Disease
AD is a multi-faceted, progressive neurodegenerative disease and the most common form of dementia, characterized by both physiological and behavioral abnormalities. It's most commonly diagnosed after a steady decline in cognitive thinking skills as well as memory loss2.In most cases, initial damage to the brain occurs a decade before symptoms become apparent3. The second stage, when most diagnoses occur, is referred to as symptomatic predementia, prodromal AD, or mild cognitive impairment (MCI). MCI is characterized by memory issues that are more severe than normal for a patient's age, such as losing items frequently, forgetting important dates or appointments, and difficulty remembering certain words4.
The diagnosis of a form of dementia, such as Alzheimer's, overcomes a diagnosis of MCI when the patient displays a significant interference in their ability to perform daily activities or function at work5.
What are the Biological Mechanisms of Alzheimer's Disease?
There are two forms of AD, each with different causes and biological mechanisms.Familial or early-onset AD is hereditary and typically occurs before age 65. Accounting for less than <5% of patients, this form of the disease is caused by dominant mutations in a few key genes. Sporadic, or late-onset AD, which is much more common, typically shows up after age 65 and is associated with both genetic and environmental factors.
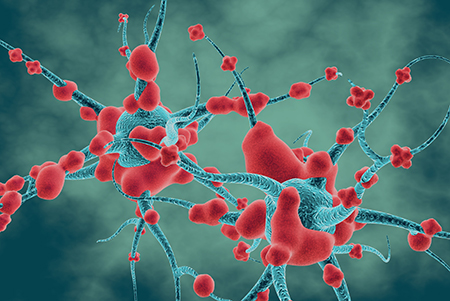
Most neurodegenerative diseases form due to the aggregation of misfolded proteins in the brain. In the case of AD, hypotheses on the biological mechanisms involved in disease formation have historically focused on two different proteins: amyloid beta (Aβ) and tau.
Aβ is a cleavage product of the mature protein amyloid precursor protein (APP) encoded by the APP gene. When mutations in APP occur, amyloid plaques form due to amyloid overaccumulation or the formation of misfolded Aβ around neurons. The fibrils that Aβ aggregate into then contribute to neuronal cell death6.
Tau is a highly soluble microtubule-associated protein (MAP) that is responsible for stabilizing microtubule formation. When tau is hyperphosphorylated, it can form less soluble, more toxic neurofibrillary tangles (NFTs), leading to the dysregulation of microtubule development7,8.
Despite research focused on these two hypotheses, the molecular links between Aβ and tau remain unclear.
Frequently, the formation of both protein aggregates begins in the hippocampus, affecting the cells that interconnect with the basal forebrain, thalamus, and hypothalamus, which are the structures essential for forming memories9. However, new evidence of peripheral inflammation indicates this process may occur outside the hippocampus region10. As the proteins spread, neurons undergo cellular death, and the overall volume of the brain tissue decreases. Additionally, Aβ plaques can block cellular signaling in the synaptic space, triggering additional inflammation and targeted phagocytosis through an activated immune response11. When compared to healthy adult controls, it has been shown that the brain scans of patients with either MCI or later stage dementia can be identified due to their decreased brain tissue size12. While the amyloid plaque and tau protein hypotheses have dominated the literature for some time, a growing body of evidence is beginning to call them into question by demonstrating the presence of other pathological drivers in the brains of patients with AD or MCI before amyloid plaques or neurofibrillary tangles develop10.
Unraveling the Risk Factors for Alzheimer's Disease
Several genes are considered conclusive risk factors for Alzheimer's disease.The APOE gene was discovered in 1993 as a risk factor primarily associated with the sporadic form of the disease. The protein produced, Apolipoprotein E (ApoE), is involved in cholesterol metabolism and cholesterol transport to cells throughout the body. Three polymorphisms are encoded by this gene—APOE2, APOE3, and APOE4—with the APOE4 allele increasing the risk of multiple diseases substantially13-16. In fact, researchers estimate that 40-65% of Alzheimer's patients have the APOE4 gene17. Investigators have hypothesized that different forms of ApoE can bind to and stabilize Aβ plaques, and that ApoE can contribute to the development of atherosclerosis, a major risk factor for Alzheimer's18,19.
In contrast, the familial, or early-onset, form of AD is most often associated with one of three single-gene mutations: amyloid precursor protein (APP) on chromosome 21, presenilin 1 (PSEN1) on chromosome 14, or presenilin 2 (PSEN2) on chromosome 1.
These mutations result in the production of proteins associated with AD, including APP, leading to amyloid plaque development.
Researchers are also finding that variants in TREM2 (the triggering receptor expressed on myeloid cells 2) may be a risk factor for AD, increasing the odds of disease development as much as three-fold. The correlation between TREM2 variants and Alzheimer's development supports the concept that immune and inflammatory pathways may contribute to the disease20.
Treatment Options for Alzheimer's Disease
Tacrine (Cognex), an acetylcholinesterase inhibitor, was the first drug to be FDA-approved for the treatment of Alzheimer's-related memory loss and cognitive impairment in 1993. Since then, several drugs have been introduced to the market and have experienced varying degrees of success in treating the cognitive problems associated with the disease, while many others are in the pipeline.Three other acetylcholinesterase inhibitors include rivastigmine, galantamine, and donepezil21,22. Additionally, memantine is an NMDA receptor agonist that acts on the glutaminergic system to prevent receptor overstimulation23. While some studies claim that there is a statistically significant improvement in cognitive symptoms for the duration of the treatment, there is no medication that can delay the onset or slow the progression of the disease.
Perhaps the most highly publicized and controversial Alzheimer's drug is Aduhelm (aducanumab), an antibody-based therapeutic that Biogen launched in July 2021 after accelerated approval by the FDA. Controversy over the drug's launch stemmed from the fact that the FDA granted approval based on evidence that it cleared amyloid plaques in clinical trial patients, as opposed to evidence of its efficacy in slowing cognitive decline24. Biogen planned to collect more real-world data on Aduhelm in a large-scale clinical trial, but the trial was terminated in June 2022 due to concerns that recent Medicare coverage policies would greatly reduce the use of the drug, significantly limiting clinical trial enrollment.
More recently, Eli Lilly applied for accelerated approval of donanemab, another amyloid plaque-targeting therapeutic, with the FDA's acceptance of the application expected by February 2023. In a limited Phase 2 trial, early symptomatic patients treated with donanemab achieved a higher composite score for cognition and scored better on performing daily activities than those on a placebo25.
As of early 2022, there were 143 agents in use in 172 clinical trials for AD therapeutics, according to ClinicalTrials.gov. Of the drugs in some phase of clinical trial, the majority (83.2%) are disease-modifying therapies, while an additional 9.8% are treatments to enhance cognitive symptoms.
Alzheimer's Research Resources
A number of resources exist to support and accelerate AD research.To expedite the rate of drug testing and approval, the Coalition Against Major Diseases established a database in 2010, which included 4,000 patients who participated in 11 industry-sponsored clinical trials of AD treatments. Researchers can access the resulting database, CAMD AD/MCI, through an online portal.
Later that year, the Alzheimer's Association introduced the TrialMatch® tool—which helps AD patients and healthy adult volunteers locate clinical studies with the goal of advancing drug development.
In 2012, the Dominantly Inherited Alzheimer Network launched the first major clinical trial of three drugs that were developed to prevent the onset of the disease in those patients who inherited an autosomal dominant mutation in the PSEN1, PSEN2, or APP genes (ClinicalTrials.gov Identifier: NCT01760005).
The US Department of Health and Human Services Alzheimer's website also provides a list of current resources for investigators studying the disease.
Rodent Models for Preclinical Alzheimer's Research
The first transgenic mouse model with Alzheimer's-like neuropathy, the PDAPP mouse, produced high levels of human mutant APP, which formed plaques and negatively affected the neural synapses similar to the disease26. In addition to the histopathology in this mouse, additional studies have displayed impaired cognitive function when performing various tasks27-28.Since the PDAPP model's introduction in 1995, many rodent models have been developed for studying the disease. The Alzheimer's Disease Forum maintains a database of 160 models and the physiological conditions each model develops over time. All rodent models are characterized based on the ages they develop each condition (including plaques, tangles, neuronal loss, gliosis, changes in long-term potentiation and long-term depression, cognitive impairment, and synaptic loss).
Taconic Biosciences offers multiple rodent models to support Alzheimer's research, with familial AD models and sporadic AD models that include three humanized apoE mouse models. And while the number of preclinical models available to support this field has increased significantly over the last several decades, the continued evolution and enhancement of both familial and sporadic models is critical for continued advancements in AD research and treatment.
Watch the Related Taconic Biosciences' Webinar:
















.jpg)

.jpg)
.jpg)
.jpg)
.jpg)





.jpg)


.jpg)
.jpg)




.jpg)




.jpg)

.jpg)



