During our Virtual NASH Symposium on August 25, Dr. Michele Vacca will present the keynote address on recapitulating translational NASH in a mouse model. Here, he draws on his distinguished career as a physician and a researcher to share insights on the challenges and opportunities of studying NASH in preclinical models.
Liver disease on the spectrum of NAFLD (non-alcoholic fatty liver disease) and NASH (non-alcoholic steatohepatitis) continues to complicate drug discovery due to the complex interplay of drivers behind its development and progression. It was that very complexity that encouraged Dr. Michele Vacca to devote much of his life's work to studying liver disease pathophysiology and exploring the preclinical models that best recapitulate it.
After completing his medical residency, Dr. Vacca decided to pursue his doctorate under the mentorship of Professor Antonio Moschetta, a renowned expert in hepatic metabolism. He was investigating the metabolic consequences of obesity, and this is where his interest in NAFLD began to flourish.
"We saw that one complication of obesity, adipose tissue dysfunction, and metabolic syndrome is absolutely NAFLD," he said. "From there, I became very interested in learning more about how adipose tissue function can influence hepatic metabolism." That led him to the University of Cambridge, where he studied NASH disease drivers with Dr. Antonio Vidal-Puig and Jules Griffen, renowned experts in obesity and lipotoxicity, and nutrition and metabolomics, respectively.
Fast forward a bit: Dr. Vacca now co-leads the preclinical team of the Liver Investigation: Testing Marker Utility in Steatohepatitis (LITMUS) project, a large-scale effort involving clinicians and researchers from across Europe and the European Federation of Pharma Industries (EFPIA). The project is helmed by Dr. Quentin Anstee (University of Newcastle), and Dr. Vacca's co-leads include Dr. Vidal-Puig and Dr. Jim Perfield (Eli Lilly). LITMUS' aims are to develop, validate, and qualify non-invasive biomarkers for NAFLD/NASH testing as an alternative to traditional liver biopsies, which can be costly and risky.
"Our group has generated the largest collection of preclinical NASH models, with the intent to develop a coherent preclinical pipeline for reverse translation of possible non-invasive NASH biomarkers," Dr. Vacca explained.
"My collaborators and I had to reverse-translate human biomarkers of the disease into animal studies to provide translatable insights, but it was not clear which models we should use," he said. Querying their LITMUS consortium colleagues, they discovered more than 100 different animal models being used among them, after factoring in sex and other variables. Looking outward, a recent metanalysis documented almost 4,000 options mentioned in the literature!
Amidst this diversity, the preclinical LITMUS group was eager to identify optimal model choices.
"Our idea was to turn this diversity, which was initially a problem, into something that is informative about modeling the disease," he said. Using bioinformatics, the preclinical group ranked 40 of the most commonly used models based on their ability to best approximate human disease burden.
"We approached the project with clinical eyes, trying to get the best translatable response from a clinical perspective," he added. "For example, our approach avoids prioritizing phenotypes that don't necessarily translate between animals and humans, like weight loss, and also considers factors known to lead to NAFLD, like metabolic syndrome, integrating this information with histology and transcriptomics."
Since every individual human dataset within a larger omics-based characterization of disease is prone to approximation--due to the composition of the study population and the histological endpoints that are especially sensitive to the "human eyes" errors (a score based on subjective rather than absolute quantification)--they used multiple human datasets showing agreement as reference. "Without a clear proxy you inevitably have a lot of variability in how you validate the translatability of models," Dr. Vacca said.
An accomplishment of the LITMUS consortium was to provide an upgrade over the existing ad-hoc scoring system for rodent liver histology that had been adapted from scoring systems applicable to humans. He cites hepatocyte ballooning as an example of a particularly unreliable endpoint needing critical analysis. The LITMUS consortium deployed digital pathology approaches and uncovered that lack of agreement around ballooning was usually even more prominent in mouse models than previously appreciated.
Also, the degree of obesity does not necessarily predict liver damage. "You might have patients who are pathologically obese but show mild liver disease; on the other hand, overweight subjects might show advanced liver disease." This complicates study design and interpretation.
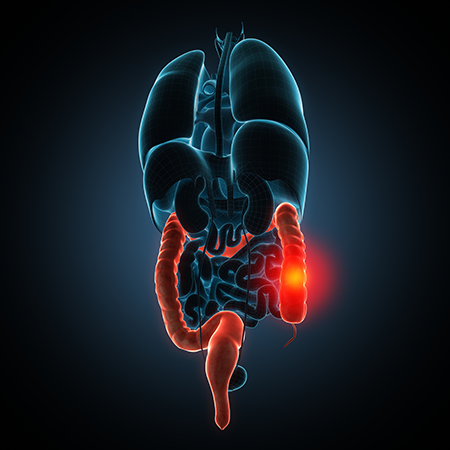
Though any preclinical model has limitations, Dr. Vacca believes in vivo models cannot be replaced yet and are currently very useful tools for NAFLD/NASH research. Metabolic syndrome and NAFLD are complex diseases arising from a dysfunctional interplay among multiple organs in addition to the liver: the gut, pancreas, brain, muscle and adipose tissues are all implicated. "If you're using a model that features the dysfunction of a single organ you might lose the whole picture of compensatory mechanisms occurring in vivo with the potential of obtaining non-translatable data," he pointed out.
Advanced in vitro models are being perfected but "it will take time to solve current limitations allowing their sole use," he said. Indeed, in vitro models mainly focus on liver function without accounting for influence from the other organs.
Dr. Vacca acknowledges that in vivo models also have their limitations, especially with regards to substantial metabolic differences among animal species and humans. True-fashioned translational projects require a combination of the two approaches.
While researchers seeking limited data about these diseases on a fast timeline still turn to mice raised on a choline-deficient diet, known to produce hepatic steatosis and inflammation, this approach models steatosis driven by a nonphysiological mechanism impacting several hepatic functions. Moreover, this approach doesn't develop the systemic context of metabolic syndrome characteristic of human NASH, so it is rarely suitable for preclinical drug development.
The LITMUS preclinical group has found that one of the modified AMLN diet mouse models produced by Taconic performs very well at recapitulating the human condition when it comes to NAFLD and NASH. "This is one of the few models to develop fibrosis in a mindful metabolic context and acceptable duration; we see gene expression, histology, and metabolic data aligning in the same direction of humans," he said.
Preclinical researchers will be able to capitalize on the LITMUS work to refine diet formulations and incorporate combinations with other variables influencing perceived disease trajectory, such as selective time points, mouse genetic backgrounds, and housing conditions. These studies are expected to "proceed in parallel with the huge investments in human multi-omics studies that are defining the pathways important to disease progression, and that will need to be confirmed as featured in mice," Dr. Vacca noted.
Liver disease on the spectrum of NAFLD (non-alcoholic fatty liver disease) and NASH (non-alcoholic steatohepatitis) continues to complicate drug discovery due to the complex interplay of drivers behind its development and progression. It was that very complexity that encouraged Dr. Michele Vacca to devote much of his life's work to studying liver disease pathophysiology and exploring the preclinical models that best recapitulate it.
After completing his medical residency, Dr. Vacca decided to pursue his doctorate under the mentorship of Professor Antonio Moschetta, a renowned expert in hepatic metabolism. He was investigating the metabolic consequences of obesity, and this is where his interest in NAFLD began to flourish.
"We saw that one complication of obesity, adipose tissue dysfunction, and metabolic syndrome is absolutely NAFLD," he said. "From there, I became very interested in learning more about how adipose tissue function can influence hepatic metabolism." That led him to the University of Cambridge, where he studied NASH disease drivers with Dr. Antonio Vidal-Puig and Jules Griffen, renowned experts in obesity and lipotoxicity, and nutrition and metabolomics, respectively.
Fast forward a bit: Dr. Vacca now co-leads the preclinical team of the Liver Investigation: Testing Marker Utility in Steatohepatitis (LITMUS) project, a large-scale effort involving clinicians and researchers from across Europe and the European Federation of Pharma Industries (EFPIA). The project is helmed by Dr. Quentin Anstee (University of Newcastle), and Dr. Vacca's co-leads include Dr. Vidal-Puig and Dr. Jim Perfield (Eli Lilly). LITMUS' aims are to develop, validate, and qualify non-invasive biomarkers for NAFLD/NASH testing as an alternative to traditional liver biopsies, which can be costly and risky.
"Our group has generated the largest collection of preclinical NASH models, with the intent to develop a coherent preclinical pipeline for reverse translation of possible non-invasive NASH biomarkers," Dr. Vacca explained.
In Search of the Best NASH/NAFLD Model
Now an assistant professor in the Interdisciplinary Department of Medicine at Università degli Studi di Bari "Aldo Moro", Dr. Vacca has played a central role in the LITMUS project's development of an unbiased, bioinformatics approach to better understanding NASH drivers and identifying the most translatable preclinical models."My collaborators and I had to reverse-translate human biomarkers of the disease into animal studies to provide translatable insights, but it was not clear which models we should use," he said. Querying their LITMUS consortium colleagues, they discovered more than 100 different animal models being used among them, after factoring in sex and other variables. Looking outward, a recent metanalysis documented almost 4,000 options mentioned in the literature!
Amidst this diversity, the preclinical LITMUS group was eager to identify optimal model choices.
"Our idea was to turn this diversity, which was initially a problem, into something that is informative about modeling the disease," he said. Using bioinformatics, the preclinical group ranked 40 of the most commonly used models based on their ability to best approximate human disease burden.
"We approached the project with clinical eyes, trying to get the best translatable response from a clinical perspective," he added. "For example, our approach avoids prioritizing phenotypes that don't necessarily translate between animals and humans, like weight loss, and also considers factors known to lead to NAFLD, like metabolic syndrome, integrating this information with histology and transcriptomics."
Since every individual human dataset within a larger omics-based characterization of disease is prone to approximation--due to the composition of the study population and the histological endpoints that are especially sensitive to the "human eyes" errors (a score based on subjective rather than absolute quantification)--they used multiple human datasets showing agreement as reference. "Without a clear proxy you inevitably have a lot of variability in how you validate the translatability of models," Dr. Vacca said.
An accomplishment of the LITMUS consortium was to provide an upgrade over the existing ad-hoc scoring system for rodent liver histology that had been adapted from scoring systems applicable to humans. He cites hepatocyte ballooning as an example of a particularly unreliable endpoint needing critical analysis. The LITMUS consortium deployed digital pathology approaches and uncovered that lack of agreement around ballooning was usually even more prominent in mouse models than previously appreciated.
A Complex Disease Requires In Vivo Models
What makes it especially challenging to understand what drives NASH and NAFLD, according to Dr. Vacca, is that they aren't black-or-white conditions. "The degree of steatosis does not linearly correlate with inflammation, cell damage or fibrosis; clustering the patients into groups is not easy and pathophysiologically it is probably the quality of fat that matters the most," he explained.Also, the degree of obesity does not necessarily predict liver damage. "You might have patients who are pathologically obese but show mild liver disease; on the other hand, overweight subjects might show advanced liver disease." This complicates study design and interpretation.
Though any preclinical model has limitations, Dr. Vacca believes in vivo models cannot be replaced yet and are currently very useful tools for NAFLD/NASH research. Metabolic syndrome and NAFLD are complex diseases arising from a dysfunctional interplay among multiple organs in addition to the liver: the gut, pancreas, brain, muscle and adipose tissues are all implicated. "If you're using a model that features the dysfunction of a single organ you might lose the whole picture of compensatory mechanisms occurring in vivo with the potential of obtaining non-translatable data," he pointed out.
Advanced in vitro models are being perfected but "it will take time to solve current limitations allowing their sole use," he said. Indeed, in vitro models mainly focus on liver function without accounting for influence from the other organs.
Dr. Vacca acknowledges that in vivo models also have their limitations, especially with regards to substantial metabolic differences among animal species and humans. True-fashioned translational projects require a combination of the two approaches.
While researchers seeking limited data about these diseases on a fast timeline still turn to mice raised on a choline-deficient diet, known to produce hepatic steatosis and inflammation, this approach models steatosis driven by a nonphysiological mechanism impacting several hepatic functions. Moreover, this approach doesn't develop the systemic context of metabolic syndrome characteristic of human NASH, so it is rarely suitable for preclinical drug development.
The LITMUS preclinical group has found that one of the modified AMLN diet mouse models produced by Taconic performs very well at recapitulating the human condition when it comes to NAFLD and NASH. "This is one of the few models to develop fibrosis in a mindful metabolic context and acceptable duration; we see gene expression, histology, and metabolic data aligning in the same direction of humans," he said.
Where NAFLD/NASH Research is Headed
Now that the LITMUS project has reviewed and ranked commonly used NAFLD/NASH options data to arrive at a consensus on the best animal models, the next phase of the project will be to reverse-validate human biomarkers to build up a coherent pipeline for translational studies and preclinical drug discovery.Preclinical researchers will be able to capitalize on the LITMUS work to refine diet formulations and incorporate combinations with other variables influencing perceived disease trajectory, such as selective time points, mouse genetic backgrounds, and housing conditions. These studies are expected to "proceed in parallel with the huge investments in human multi-omics studies that are defining the pathways important to disease progression, and that will need to be confirmed as featured in mice," Dr. Vacca noted.











.jpg)

.jpg)
.jpg)
.jpg)
.jpg)



.jpg)


.jpg)
.jpg)

.jpg)


.jpg)





.jpg)

.jpg)


