Laura Griffin, PhD
Revisiting the Humanized NOG-EXL: A Preclinical Model for Cell Therapy Applications
Thursday, September 21, 2023

By definition, cell therapy is the transfer of autologous or allogeneic cellular material into a patient for medical purposes. Although the technique was first explored in the late 19th century, it has only recently gained traction as a standard of care in the medical field. Global market share is estimated to expand from $9.5 billion in 2021 to $23 billion in 20281. With respect to immuno-oncology applications, the major models of cell therapy under investigation include tumor-infiltrating lymphocytes (TILs), T cell receptor (TCR) modified T cells, and chimeric antigen receptor (CAR) engineered cells (CAR-T, CAR-NK, etc.). TIL therapy involves selecting and activating tumor-infiltrating T cells extracted directly from patient tumors and infusing them back into the host. In contrast, CAR and TCR modified T cell therapies involve acquiring lymphocytes of interest from a patient's peripheral blood, genetically engineering them to recognize and target tumor antigens, and finally infusing them back into the host2.
To date, CAR-T therapies targeting B cell malignancies comprise the vast majority of genetically modified cell-based therapies with US Food and Drug Administration approval. Despite success in this category, much work remains for the development of CAR therapies targeting non-B-cell malignancies. More sophisticated approaches are needed to overcome tumor-defense mechanisms such as immunosuppression or physical barriers to entry into solid tumors3.Complex therapeutic techniques require advanced preclinical models for evaluation that should be selected with care.
Humanized Immune System Mice for Cell Therapy Evaluation
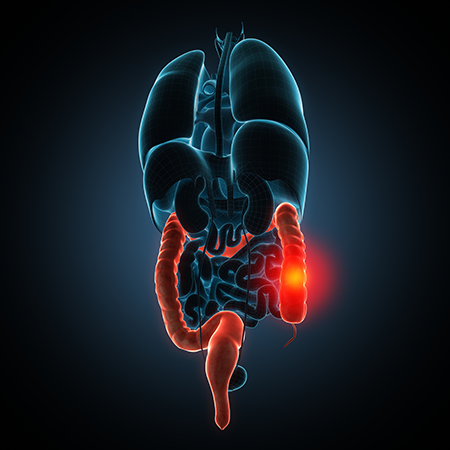
Super immunodeficient mice, such as the NOG-EXL, are powerful tools for preclinical evaluation of immuno-oncology therapeutics. Given that they can be engrafted with human cells like [CD34+] hematopoietic stem cells (HSCs) and human tumors, it is possible to study the interaction of immuno-oncology therapies with the human immune system and the tumor milieu. NOG-EXL mice are also exceptionally powerful assets in the preclinical arsenal in that they support the expansion of both myeloid and lymphoid cell lineages when engrafted with HSCs. This is possible due to the transgenic expression of two human signaling molecules: interleukin-3 and granulocyte-macrophage colony stimulating factor4.
When evaluating cell therapy applications preclinically, oftentimes a super immunodeficient model (such as the hIL-2 NOG for CAR-T therapy or hIL-15 NOG for CAR-NK therapy) is used without the additional element of an engrafted human immune system. While this approach can be beneficial to understand how the drug modality interacts with the tumor, it largely ignores the potential interaction with the rest of the immune system. Evaluating cell therapies in the context of both the innate and adaptive immune compartments with humanized NOG-EXL mice can offer perspective in this regard and quite possibly hint at translatability in the clinic.
Humanized NOG-EXL for evaluation of CAR-T and CAR-Macrophages
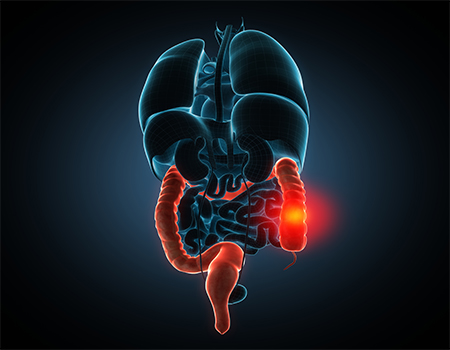
Last year, two studies utilizing a humanized NOG-EXL model for the evaluation of innate and adaptive cell therapies were published, which showcase the utility of this preclinical model for cell therapy as well as combination therapies. In the first publication by Cao et al., a novel CAR-T therapy was evaluated alone and in combination with microwave ablation (MWA) therapy in humanized NOG-EXL mice engrafted with a non-small cell lung cancer, A5495. Cell therapies targeting solid tumors have not been as successful as those targeting hematological cancers in early clinical trials, due to factors such as insufficient infiltration of CAR-T cells and the immunosuppressive tumor microenvironment (TME), to name a few. In contrast, MWA has been successfully employed in the clinic to treat solid tumors of multiple origins. The electromagnetic waves produced by MWA generate heat, leading to hyperthermic lethal or sublethal injury to ablated cells of the TME. However, local tumor residue and marginal recurrence are common due to incomplete ablation. The shortcomings of these two therapies led Cao et al. to hypothesize that combining MWA and CAR-T cell therapies could be a powerful combination for treating and eliminating solid tumors in vivo, and accordingly developed an AXL-targeted CAR-T therapy. AXL is a typical oncogene that is over-expressed in many cancers and is typically correlated with poor prognosis.
Results from the study demonstrated that both the CAR-T therapy and MWA were able to suppress tumor growth when administered as monotherapies, but combination therapy exerted a greater antitumor response, reaching nearly complete ablation after three weeks of treatment. Moreover, combination therapy allowed for greater infiltration of CD3+ cells into the TME compared to the monotherapies and more importantly, the MWA therapy appeared to significantly improve CAR-T cell penetration into the TME. A significant reduction in pro-tumor M2 macrophages was also observed for the AXL-CAR-T monotherapy and to a greater extent than the combination therapy, indicating a beneficial reprogramming of the TME due to treatment. Additionally, there were no signs of organ toxicity and altogether, these results suggest that combining MWA with CAR-T could be a useful technique to improve CAR-T efficacy when applied to solid tumor malignancies.
In a separate publication by Chen et al. a CAR-macrophage therapy for glioblastoma multiforme (GBM) relapse was evaluated using humanized NOG-EXL mice6. GBM is the most intractable malignant brain tumor in adults, and despite the use of aggressive multi-modality treatments, most GBMs recur around the initial resected cavity within 8-12 months after resection. Macrophages and resident microglia are abundant cell types in the GBM, many of which are removed in tumor debulking events, however the resultant inflammation induced by surgery often leads to enrichment of immunosuppressive-type macrophages and microglia around the tumor cavity, resulting in tumor recurrence. The researchers therefore hypothesized that genetically engineering intracavitary macrophages could potentially redirect phagocytic activity, functioning as antigen presenting cells to stimulate an adaptive immune response to assist in the prevention of relapse. The researchers planned to test this hypothesis using a PDX model and humanized mice.
In order to study GBM recurrence, the researchers established an orthotopic GBM model in humanized NOG-EXL mice by injecting patient-derived glioblastoma cells and allowing them to grow for 12 days. PDX glioblastomas were then surgically removed, and CAR-macrophages were applied into the resection cavity in combination with anti-CD47 antibodies. The CAR-macrophages ablated residual glioblastomas that remained by phagocytic activity and stimulating an adaptive immune response; increased CD8+ and CD4+ T cells, M1 macrophages, and dendritic cell populations in the surgical cavity, were reported following therapy. Additionally, 83% of treated mice survived over 90 days following invasive surgery and treatment without tumor resurgence, demonstrating efficacy of the treatment as well as resilience of the model for invasive, complex, and longstanding treatment paradigms.
Conclusion
The studies discussed above demonstrate that humanized NOG-EXL mice from Taconic Biosciences are an excellent tool for evaluating novel techniques in this field, as they are able to:
- Allow for evaluation of cell therapies in the context of a more complete and realistic human immune system compared to other super immunodeficient models, as this model supports both innate and adaptive immune cell persistence
- Support successful engraftment of PDX at disease-relevant organ sites
- Demonstrate efficacy for diverse types of mono and combination therapies
- Support a long study window even following significant and invasive manipulation
If you want to learn more about using this powerful model for a new immuno-oncology application, contact a Taconic Biosciences Field Application Scientist today.











.jpg)

.jpg)
.jpg)
.jpg)
.jpg)



.jpg)


.jpg)
.jpg)

.jpg)


.jpg)





.jpg)

.jpg)




