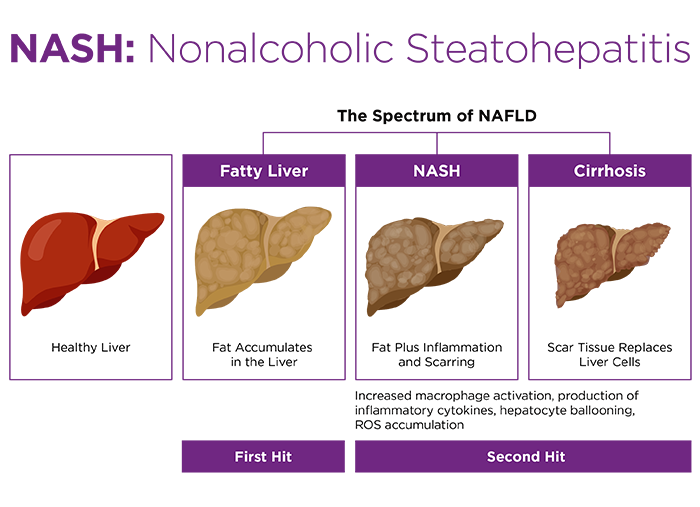
According to Younossi et al., "NAFLD is one of the most important causes of liver disease worldwide and will probably emerge as the leading cause of end-stage liver disease in the coming decades, with the disease affecting both adults and children1".
The Silent NAFLD Epidemic
NAFLD has been compared to a silent epidemic, and incidence is increasing. "NAFLD is known to be highly associated with several metabolic conditions...Thus, it is expected that the incidence of NAFLD should rise in parallel to the increasing incidence of obesity and "[type 2 diabetes mellitus]"1."There are few symptoms until disease is quite advanced. According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), "Usually, nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH) are silent diseases with few or no symptoms. You may not have symptoms even if you develop cirrhosis due to NASH".
How NASH is Diagnosed
The gold standard for NASH diagnosis is a liver biopsy. Liver enzymes are sometimes normal in people with NAFLD. While ultrasound can detect fatty liver, it cannot detect fibrosis or inflammation2.No Approved NASH drugs
There are currently no approved therapeutics for NAFLD, so treatment focuses on weight loss and lifestyle changes. Advanced liver disease may require a liver transplant. With a large and growing patient population and no approved therapeutics, pharma and biotech are investing heavily in NAFLD/NASH research.Therapeutic goals are segmented based on different aspects of the disease, such as reducing inflammation, reversing fibrosis, or stabilizing cirrhotic patients. Preclinical research is also thus segmented, with different animal models used depending on the particular NAFLD phenotype under investigation.
NAFLD/NASH Animal Models
Preclinical animal models for NAFLD and NASH can be divided into three classes: diet-induced models, chemically-induced models, and genetic models.Diet-induced NAFLD models
Mice fed a diet deficient in methionine and choline develop hepatic fat accumulation, inflammation and fibrosis, but do not become obese and thus do not represent all aspects of systemic NAFLD disease. Diets with various combinations of high fat, high fructose and/or high cholesterol have been widely used to model NAFLD. For example, diet-induced obese C57BL/6 mice readily develop steatosis, but do not appear to develop more advanced NASH phenotypes.The Amylin liver NASH model (AMLN) combines high fat, high fructose and high cholesterol in a single diet. C57BL/6 mice fed the AMLN diet become obese, get fatty liver and develop liver inflammation and fibrosis after 26+ weeks on diet, with inter-animal variability observed for development of the inflammation and fibrosis phenotype3,4.
One challenge with diet models can be prolonged conditioning time required prior to start of studies. Availability of pre-conditioned mice from animal vendors can dramatically accelerate the start of NASH studies.
Chemically-induced NAFLD models
Low dose streptozotocin administration, combined with a high fat diet, has been used to model NAFLD in mice, with steatosis, inflammation, fibrosis and even hepatocellular carcinoma resulting. Administration of carbon tetrachloride (CCl4) is commonly used to induce liver fibrosis, alone or with co-administration of high fat diet3.Genetic models
Ob/ob mice develop obesity and steatosis, but require additional conditioning in the form of diet or chemical induction to progress on to NASH phenotypes3. Apoe knockout mice, which are commonly used for atherosclerosis research, can develop NASH phenotypes such as steatosis, inflammation and fibrosis when fed a high fat, high cholesterol diet5.Although genetic and chemically-induced models may not be relevant in terms of the mechanism of disease induction, their advantage can be more rapid disease induction. High fat diet models are typically slower, but may better model the full spectrum of NAFLD and co-morbid metabolic disease. This list of models is by no means exhaustive and review articles may be consulted for additional information.











.jpg)

.jpg)
.jpg)
.jpg)
.jpg)



.jpg)


.jpg)
.jpg)

.jpg)


.jpg)





.jpg)

.jpg)




